Comedonal Acne – Complete Guide | AcneSkinGuide
Summary of Comedonal Acne
Comedonal acne, characterized by whiteheads and blackheads, is a non-inflammatory yet frustratingly persistent type of acne. It occurs when hair follicles become clogged with excess oil, dead skin cells, and bacteria. Multiple factors contribute, including hormonal changes, oily skin, comedogenic makeup/skincare products, medications, and potentially diet. While lacking inflammation initially, untreated comedonal acne can progress into more severe inflammatory acne with increased scarring risk.
Treatment involves over-the-counter topicals like salicylic acid and benzoyl peroxide, prescription retinoids or antibiotics, and procedures like extractions. However, prevention through a tailored skincare routine, avoiding pore-clogging products, and gentle exfoliation is crucial for long-term management. Despite being “milder,” comedonal acne poses risks like darkening of blackheads, potential scarring from improper extraction, and confidence issues, especially in adolescents. With patience, proper treatment, and realistic expectations, this stubborn condition is manageable.
Our Top 3 Recommended Acne Treatment Products

#1 Paula's Choice Acne Treatment
The 3-step kit features a cleanser and exfoliating solution with 2% salicylic acid, as well as a 5% benzoyl peroxide treatment that effectively treats even severe acne, though the benzoyl peroxide can be drying. The kit delivers serious results for stubborn acne, despite its slightly higher price point compared to drugstore options. Check The Price Now

#2 EMUAID Overnight Acne Treatment
The EMUAID Overnight Acne Treatment features a two-phase solution, with an exfoliating first step to unclog pores and an intensive treatment gel that rapidly reduces inflammation, redness, and swelling of even severe, cystic breakouts, despite a slightly medicinal scent and higher price point compared to other options. Check The Price Now

#3 Differin Acne Treatment
The Differin 0.1% adapalene gel normalizes cell turnover and unclogs pores to effectively treat acne, though it requires 2-3 months of consistent use with an adjustment period of dryness and purging before seeing maximum results, which are worth the effort for clearer, more even-toned skin. Check The Price Now
Understanding Comedonal Acne: The Stubborn Blemish
Acne is one of the most common skin conditions, affecting millions worldwide. While many are familiar with inflamed pimples, comedonal acne is a specific type that warrants attention. These pesky whiteheads and blackheads may seem harmless but can be frustratingly persistent and lead to further issues if not properly managed.
What Exactly is Comedonal Acne?
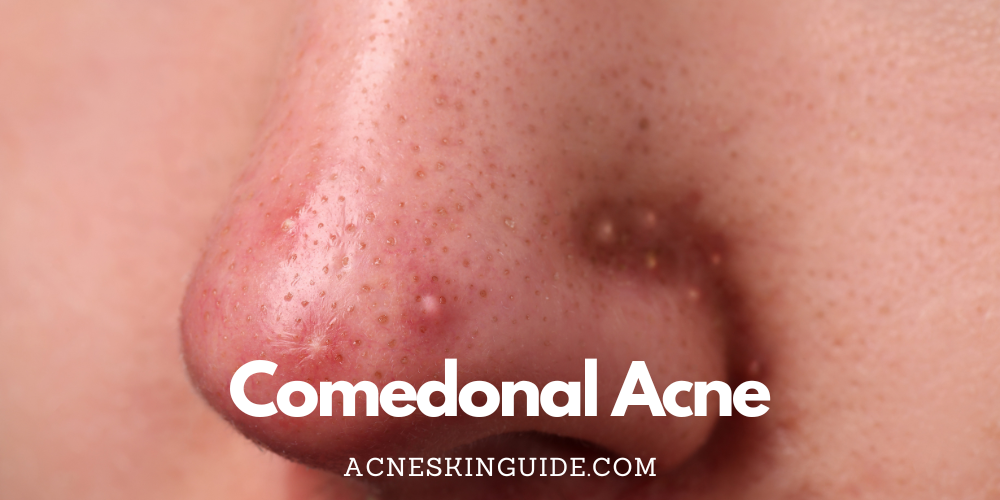
Comedonal acne, also known as non-inflammatory acne, involves clogged hair follicles or pores that become plugged with excess oil (sebum), dead skin cells, and bacteria. When this plug stays beneath the skin’s surface, it forms a whitehead or closed comedo. If the plug protrudes from the pore and is exposed to air, it oxidizes and forms a blackhead or open comedo.
While seemingly less severe than red, inflamed pimples, comedones can be equally frustrating and persistent. If not treated properly, they can develop into more serious forms of acne like papules, pustules, nodules, and cysts.
Causes and Contributors
Multiple factors influence the development of comedonal acne. Excessive oil production, often triggered by hormonal changes during puberty, is a leading culprit. However, hormonal imbalances can affect people of any age.
Those with naturally oily or acne-prone skin types may be more susceptible. Using heavy, oil-based makeup and skincare products that clog pores (comedogenic) can exacerbate the problem. Even certain medications like lithium, corticosteroids, and anabolic steroids may lead to increased comedones.
While research is ongoing, some studies suggest diet may play a role, with higher intake of dairy, sugary foods, and refined carbs potentially worsening acne.
Differentiating From Other Types
The key distinction between comedonal acne and other forms is the lack of inflammation. Whiteheads and blackheads develop without the red, swollen bumps characteristic of inflammatory acne like papules (red, tender bumps), pustules (pus-filled lesions), or nodules/cysts (deep, painful breakouts).
However, leaving comedonal acne untreated can eventually lead to inflammation as the plugged follicle ruptures under the skin.
Treatment Approaches
Topical products are the first line of defense against comedonal acne. Over-the-counter treatments containing ingredients like salicylic acid, retinoids (adapalene, tretinoin), and benzoyl peroxide help unclog pores and slough off dead skin cells.
For more severe or persistent cases, dermatologists may prescribe stronger retinoids, antibiotics, or hormonal therapies like birth control pills or spironolactone.
In-office procedures like comedone extractions done by an experienced professional can manually remove stubborn whiteheads and blackheads safely. Professional facials with exfoliation and extractions also provide deep cleansing.
Physical removal methods like pore strips or comedone extractors may be tempting but pose risks of scarring and infection if not used properly.
Prevention Trumps Treatment
While treatment can help reduce existing comedones, prevention is key to managing comedonal acne long-term. A consistent skincare routine tailored to your skin type is crucial.
Use gentle, non-comedogenic cleansers and lightweight oil-free/non-acnegenic moisturizers suited for acne-prone skin. Avoid heavy, greasy makeup and products containing pore-clogging ingredients like isopropyl myristate, lauric acid, and myristyl alcohol.
Regular, gentle mechanical and chemical exfoliation helps slough off dead cells before they can clog pores. Habits like removing makeup before bed and avoiding picking/squeezing also go a long way.
Downsides and Risks
While seemingly milder than inflamed pimples, comedonal acne brings its own challenges. Persistent blackheads can lead to inflammation and dark spots from the oxidized plugs. Squeezing comedones incorrectly risks scarring and potential infections.
Attempting to remove deep, stubborn blackheads or large areas of whiteheads can damage the skin if not done by a professional. Those with severe or widespread comedonal acne may develop low self-esteem and confidence issues, especially during crucial years like adolescence.
If left unchecked, comedones can progress into more serious inflammatory acne with painful cystic lesions and increased risk of scarring. Early, consistent treatment helps prevent this.
While medical treatments provide potent solutions, some topical products and procedures pose risks like excessive dryness, peeling, redness, and irritation if not used as directed.
Living in Confidence
With patience and the right approach, comedonal acne is manageable. Don’t let the seemingly harmless bumps last indefinitely. Work closely with a dermatologist to develop a tailored regimen that tackles both existing and future comedones.
Maintaining realistic expectations while embracing a comprehensive strategy of treatment and prevention will allow you to face each day confidently despite the occasional blemish. After all, clear skin starts with consistency and care for your unique and beautiful complexion.
FAQs and Answers
Can hormonal birth control help treat comedonal acne?
Yes, hormonal birth control can often help treat comedonal acne (as well as other types of acne) in women. Here’s how it works:
The hormones in birth control pills, particularly the progestin component, help reduce androgen levels in the body. Androgens like testosterone contribute to excess oil/sebum production, which allows comedones (blackheads/whiteheads) to form.
By suppressing androgen activity, birth control reduces the stickiness of skin cell contents inside pores, preventing them from becoming clogged as easily. This makes existing comedones less severe and prevents new ones from forming.
The estrogen in birth control pills also increases production of sex hormone binding globulin (SHBG), which binds to and metabolizes circulating androgens, further reducing their effects.
Some birth control formulations are FDA-approved specifically for treating acne due to their superior ability to regulate hormone levels. Examples are Yaz, Ortho Tri-Cyclen, and Estrostep.
However, it can take 2-3 months of consistent use before birth control’s effects on acne are noticeable. The ideal candidate is someone whose acne flares up cyclically around their period. Not all women see improvement, as hormones aren’t the only acne trigger.
So in summary, hormonal birth control is an effective treatment option for many women struggling with comedonal or hormonal acne by regulating internal androgen levels.
What is the role of stress in comedonal acne?
Stress can play a significant role in contributing to and exacerbating comedonal acne. Here’s how stress impacts comedonal acne:
- Increases sebum/oil production
When under stress, the body releases more androgenic hormones like testosterone which stimulate the sebaceous glands to produce more sebum or oil. This excess oil can clog pores and create an environment ripe for comedones (blackheads and whiteheads) to form. - Inflammation
Stress triggers the release of inflammatory molecules like cytokines, neuropeptides and hormones like cortisol. This inflammatory response can make existing comedones more inflamed, red and irritated. - Delays skin cell turnover
Stress disrupts the normal shedding of skin cells lining the pores. Cells can get sticky and accumulate, mixing with oil to clog follicles and create new comedones. - Compromises skin barrier
High stress weakens the skin’s protective barrier, allowing more irritants, bacteria and allergens to penetrate and further clog pores. - Hormonal fluctuations
Stress can worsen hormonal imbalances that are a primary trigger for acne, leading to increased comedonal breakouts.
Managing stress through techniques like meditation, exercise, counseling or yoga can help reduce comedonal flare-ups in acne-prone individuals. Lowering stress allows better hormonal regulation and skin cell turnover.
So while stress alone doesn’t directly cause comedonal acne, it creates an internal environment that promotes comedone formation and exacerbates existing ones. Keeping stress in check is important for clear skin.
Are there any natural remedies or home remedies for comedonal acne?
Yes, there are several natural and home remedies that some people find helpful for treating and preventing comedonal acne like whiteheads and blackheads. However, it’s important to note that their effectiveness can vary and they may not work for everyone. Here are some popular options:
- Tea Tree Oil – This essential oil has natural antibacterial and anti-inflammatory properties. Diluting tea tree oil with a carrier oil and applying it topically may help dry out whiteheads and unclog pores.
- Honey – Raw honey contains antioxidants and natural antibacterial compounds. Using a honey face mask or spot treatment can gently exfoliate and fight acne-causing bacteria.
- Green Tea – Green tea is rich in antioxidants called polyphenols that may help reduce oil production and inflammation in pores. Using cooled green tea as a toner can be beneficial.
- Apple Cider Vinegar – The acidic nature of ACV helps break down and dissolve oil and dead skin cells in clogged pores when used as a diluted toner.
- Baking Soda – Baking soda is a mild abrasive that can help physically exfoliate and remove blackhead plugs when used as a face scrub.
- Clay Masks – Different clays like bentonite and kaolin can absorb excess oil and draw out impurities from clogged pores.
- Witch Hazel – This astringent plant extract can help tighten pores and remove oil/debris when used as a toner.
While gentle and natural, these remedies may not be strong enough for severe or persistent comedonal acne. They work best as complementary treatments alongside standard medical therapies prescribed by a dermatologist.
How does exercise impact comedonal acne?
Exercise can have both positive and negative impacts on comedonal acne. Here’s a breakdown:
Potential Benefits:
- Reduces stress – Exercise helps lower stress levels, which can minimize hormonal fluctuations that trigger excess oil production and clogged pores.
- Improves blood circulation – Better circulation brings more oxygen and nutrients to the skin, which can aid in skin cell turnover and prevent pore blockages.
- Flushes out toxins – Sweating during exercise helps expel toxins and bacteria from pores that could contribute to acne.
- Boosts mood – The endorphins released during exercise can improve mood and reduce stress/anxiety, which are comedonal acne triggers.
Potential Drawbacks:
- Occlusion from sweating – Sweat, oil, dirt and bacteria can mix and become trapped in pores during exercise, leading to new comedones.
- Friction from equipment/clothing – Rubbing from tight exercise clothing, helmets, etc. can worsen existing comedones and cause new ones.
- Excessive cleansing post-workout – Over-scrubbing to remove sweat can strip away protective oils and disrupt the skin barrier.
- Increased androgens – Intense exercise may temporarily raise androgen levels in some people, stimulating more oil production.
To minimize negatives, it’s important to properly cleanse sweaty skin after workouts, wear loose, breathable fabrics, and avoid picking at any new blemishes. Keeping up with regular medical treatments is also advisable.
Overall, moderate exercise has more benefits than risks for comedonal acne when proper hygiene is followed. But individual factors like workout intensity, genetics and hormones play a role as well.
At what age does comedonal acne typically start and when does it resolve?
Comedonal acne, characterized by whiteheads and blackheads, typically follows a predictable age pattern:
Onset:
Comedonal acne most commonly begins during puberty, usually between the ages of 10-13 for girls and 12-16 for boys. This is due to the surge of hormones like androgens that increases oil/sebum production and clogs pores.
Peak Years:
Comedonal acne tends to be most severe and widespread during the mid-to-late teen years, around ages 15-19. This is when hormones are most dramatically fluctuating.
Early 20s:
Many people continue to experience persistent comedonal breakouts into their early 20s as hormones gradually stabilize after adolescence.
Potential Resolution:
For most individuals, comedonal acne starts improving by the mid-to-late 20s as hormones level out. However, it’s not uncommon for some people, especially women, to continue experiencing hormonal comedonal flare-ups into their 30s and beyond.
Factors like genetics, hormonal conditions like PCOS, stress levels, skincare routines and medications can all influence how long comedonal acne persists for each person.
While it typically originates in the teen years, adult-onset comedonal acne can also occur when triggered by hormonal changes from pregnancy, birth control, menopause or other underlying medical issues.
So in summary – comedonal acne most commonly starts around puberty, peaks in the late teens, and resolves gradually by the mid-to-late 20s for the majority, but can potentially last decades for some individuals. Early treatment helps control its course.